Osteoarthritis - Less Knee Pain, More life

Symptoms of Osteoarthritis of the Knee
Osteoarthritis of the knee (short: knee OA) is a wear disease on the knee joint. It is incurable and leads to progressive changes in the knee. In the initial stage of osteoarthritis, there is no pain or only phases of pain and restrictions in movement. With advanced osteoarthritis of the knee, pain and discomfort can increase. Most people develop wear-related osteoarthritis during the course of life. Risk factors such as obesity, joint malposition, lack of exercise, overloading and incorrect loading of the joints in some types of sports or injuries accelerate joint wear and tear and can also promote the development of osteoarthritis in young people.
Osteoarthritis changes the knee joint
As a degenerative joint disease, osteoarthritis of the knee typically starts with signs of wear and/or tiny damage in the joint cartilage. As time passes, the cartilage surface becomes rough and uneven. The joint no longer moves smoothly. It snags and grinds. Increasing friction leads to painful inflammation in the knee and fluid is effused into the joint capsule. In this condition, also referred to as activated osteoarthritis, there is constant pain. In the advanced stage of osteoarthritis, cartilage damage increases and all tissues involved in the joint are affected. The bones form spurs (osteophytes) to stabilise the joint, but cause ankylosis in the process. Knee pain occurs at increasingly shorter intervals and becomes more severe over time.

1 results out of 1
The vicious circle of osteoarthritis
Patients with osteoarthritis of the knee frequently get caught in a vicious circle:
To get relief for a painful knee, the affected person exercises less and adopts a compensatory posture. However, restricting movement only provides short-term relief from pain. In the long run, lack of exercise accelerates cartilage wear and increases pain in the knee. The affected person rests their knee even more often instead of exercising it, and the vicious circle closes.
Furthermore, the unnatural posture taken to relieve pain also causes other joints such as the hips to be overloaded, which can cause permanent damage.
Initial symptoms of osteoarthritis of the knee
The sooner osteoarthritis of the knee is recognised and counteracted, the better the chances are for getting knee pain under control, maintaining joint mobility for a long time and slowing down the progressive changes in the knee joint. If the following symptoms occur repeatedly in your knee, you should have it examined by an orthopaedist:
Knee pain after rest (start-up pain)
Knee pain after unusual exertion
Knee pain with certain movements
Knee stiffness
Grinding and crackling of the knee joint
Swelling and inflammation in the knee

Diagnosis and therapy for osteoarthritis of the knee
If your knee pains or its functions are limited, you should have it examined by an orthopaedist.
What are the symptoms of osteoarthritis of the knee?
There are a number of symptoms which are typical for osteoarthritis of the knee. They can occur individually or in combination. Depending on the level of joint wear, symptoms may be more or less severe. While symptoms of osteoarthritis of the knee are hardly noticeable – or even absent – in the early stages, patients complain of increasing pain and increasingly restricted mobility as the disease progresses. You can take preventive measures to avoid reaching this stage. These include a healthy and balanced diet, and regular activity and sports. Due to the fact that symptoms do not occur straight away, osteoarthritis of the knee often remains undetected for a long time. The first indications of osteoarthritis of the knee become apparent during everyday activities. Joints crackle and grate; climbing stairs and carrying heavy objects causes knee pain. If you observe these symptoms, you should see your doctor and ask to be examined. Doctors can use several methods to determine if your symptoms are caused by osteoarthritis of the knee.
Causes of osteoarthritis
Osteoarthritis of the knee can have many causes. The biggest risk factor for osteoarthritis of the knee is too much strain on the knee joints. Lifting and carrying heavy objects or moving wrongly can place severe strain on your joint cartilage and result in progressive wear and tear. Because they are heavier, people who are overweight place a higher load on their cartilage. This leads to an increased risk of osteoarthritis of the knee. Naturally, age also plays a significant role in the development of osteoarthritis. Cartilage loses elasticity with increasing age and can no longer regenerate as easily as in earlier years, which is why the joint disorder most frequently affects people aged 60 years and over. Nonetheless, young people are most certainly not immune to osteoarthritis of the knee! Genetic predisposition can lead to an early occurrence of the disease. Moreover, joint malalignment (knock knees or bow legs, for example) speeds up the progression of the disease. Accidents or sports injuries which affect the knee joint can also trigger the development of osteoarthritis. These include or meniscus injuries. Osteoarthritis develops slowly, so there is often a period of several years between the early stage and severe osteoarthritis. During this time, symptoms intensify gradually as wear and tear increases.
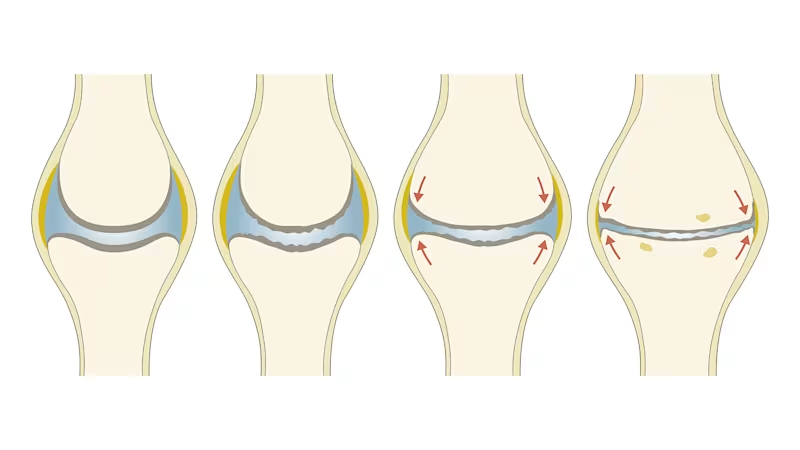
Disease progression: Stages of osteoarthritis
Osteoarthritis of the knee is classified into four degrees of severity:
Osteoarthritis degree 1:
The joint cartilage has invisible signs of wear. It is less elastic than healthy cartilage and cannot recover well after being subjected to load. Initial knee pain may occur under high load.
Osteoarthritis degree 2:
The cartilage tissue becomes thinner. The cartilage surface becomes rough and uneven. The bones form initial spurs (osteophytes). The knee is considerably less able to bear weight. At this stage of osteoarthritis, the progression of the disease can be effectively slowed by exercises, weight loss and medical devices such as braces.
Osteoarthritis degree 3:
The cartilage has partly disappeared so that the bones begin to rub against each other in some places. X-rays show pronounced bone spurs and narrowing of the joint space. At this advanced stage, osteoarthritis causes considerable movement restrictions and knee pain.
Osteoarthritis degree 4:
The joint space has narrowed considerably and the joint cartilage has almost completely disappeared. The bones are often damaged. The joint is deformed and often inflamed. In this final stage, joint-replacement surgery – i.e. a prosthetic knee joint – may be the best solution.
Diagnosing osteoarthritis of the knee: How a doctor detects joint wear
Diagnosing osteoarthritis of the knee: How a doctor detects joint wear
If you frequently suffer from knee pain and other symptoms, you may have developed osteoarthritis of the knee. To get to the bottom of the symptoms, you should see a doctor. Only a medical specialist – using a range of examinations – can determine if your symptoms are actually caused by gonarthrosis (osteoarthritis of the knee). In order to get a better overall picture, your doctor will first ask you about your general state of health and existing physical problems. Here it's absolutely essential to be honest! Tell your doctor about any and every physical anomaly you've observed over the past days or weeks. This will enable your doctor to assess if you really have osteoarthritis of the knee, or if your symptoms are perhaps caused by another disease.
Once your doctor has finished asking questions, they will generally turn their attention to the affected joint. Using palpation, they will see how sensitive you are to pressure. They will also look closely at visual anomalies such as swelling, joint effusions and axial malalignment (knock knees or bow legs) to determine whether symptoms are caused by osteoarthritis of the knee. Additional examinations will be required before your doctor can confirm the diagnosis. X-rays are generally used for this purpose. An expert can use X-ray images to determine whether joint cartilage displays irregularities or cracks, or whether osteophytes (bone spurs) have formed. The doctor can also refer you for a CT, MRI or ultrasound examination. Depending on the method used, doctors can detect bone changes, damage to the meniscus or cruciate ligament, and irregularities in the cartilage of your knee joint.

Diagnosing osteoarthritis of the knee
When talking to the physician, you should give a detailed description of your knee problems and answer the physician's questions precisely. In addition to the knee disorder, other health information such as osteoarthritis in other joints, injuries, infections or chronic diseases may also be relevant to knee pain. While performing the examination, the physician will look at the knee and check its functions. He will then x-ray it to see if any visible changes have already developed in the joint. In some cases, further examinations will be necessary to reach a diagnosis. Depending on the case, these include, for example, examinations of the blood or the joint fluid as well as other imaging procedures.

Therapy for osteoarthritis of the knee
There are three basic treatment methods for osteoarthritis of the knee: conservative (non-invasive) therapy, invasive joint-preserving therapy and invasive joint-replacing therapy. The term invasive is used for all treatments in which the doctor makes changes to the knee joint.
Conservative (non-invasive) therapies:
Conservative therapy for osteoarthritis of the knee includes all non-invasive treatments. Conservative therapy is made up of building blocks (modules).
The modules of conservative therapy for knee arthrosis include:
Wearing supports and braces
Therapeutic exercise
Special gymnastics
Light to medium sporting activity
Healthy nutrition
Weight reduction in the case of overweight
Heat and cold treatments as required
Pain-relieving ointments and gels
Analgesics and anti-inflammatory medication
Invasive joint-preserving therapies:
To relieve inflammation and pain in the knee, the physician can inject medication directly into the joint. Hyaluronic acid is frequently used as an active ingredient. Hyaluronic acid occurs naturally in healthy joints. It serves as a nutrient solution for the cartilage and is a natural lubricant for the joint. Malpositioned legs that lead to osteoarthritis can be corrected by surgically realigning the bones (corrective osteotomy).
In certain cases, an endoscopic technique is also used for joint-preserving therapy of osteoarthritis. This procedure is referred to as "arthroscopy" (joint endoscopy). However, because the success of arthroscopy is limited, it is no longer recommended as the sole treatment for osteoarthritis of the knee.
Invasive joint-replacing therapies:
If conservative or invasive joint-preserving therapies no longer provide relief of pain or improve the knee function, joint-replacing therapy should be considered. During this surgical procedure, the natural joint is replaced either fully or partially by a prosthesis (endoprosthesis/ prosthetic knee joint).

Braces can relieve knee pain
Knee or lower-leg-foot-braces, such as the Agilium Freestep, specifically relieve the painful areas in the knee joint and can provide sustainable relief from knee pain. This is also confirmed by studies. In many cases of osteoarthritis of the knee, braces can help to discontinue the use of analgesics or the dose of medication can be reduced. Side effects from the medication are effectively avoided or reduced. Knee or lower-leg-foot-braces enable patients with osteoarthritis of the knee to move around and do sports largely without pain. It is thus possible to break the vicious circle of pain, lack of exercise and progressive deterioration of the osteoarthritis.
Quote Dr Stinus: "Most of my patients are very happy with the new brace. More than half of them have been able to avoid surgery so far.”

Treading new paths with braces from Ottobock
Have a look at experiences made by patients with osteoarthritis of the knee and how they are treading new paths with Ottobock braces.

Braces from Ottobock: Solutions for different knee problems
Ottobock has developed precisely fitting braces for different knee problems. Get an overview of the range of Ottobock braces for osteoarthritis of the knee. By means of simple questions, Agilium Select takes just a few minutes to determine which brace fits your knee problem and your lifestyle.

How can osteoarthritis be treated?
Active against osteoarthritis
Osteoarthritis of the knee cannot be cured, but you can effectively alleviate pain and discomfort and significantly improve your quality of life if you actively counteract osteoarthritis by means of conscious nutrition and adapted exercise.
Nutrition
Your meals should primarily consist of fruit and vegetables, salads, plant oils, nuts and seeds. Fish like mackerel, salmon and herring are rich in nutrients and Omega-3 fatty acids that curb inflammation. Healthy fish can therefore be served twice a week. Some spices not only improve the taste of food, they are also good for the joints: turmeric, nutmeg, cinnamon and coriander have an anti-inflammatory and decongestant effect. Chilli and ginger help to relieve pain. Meat can be eaten in moderation, but poultry is preferable. Beef and pork should rarely be consumed. It is best to avoid high-sugar and high-fat processed convenience foods and to avoid alcohol and nicotine. In case of overweight, losing weight will take the strain off your joints and help you have less knee pain and feel lighter and fitter overall.

Exercise in everyday life
Regular exercise is essential to counteract the progressive changes caused by osteoarthritis, maintain knee function and relieve pain. It is important to integrate more exercise into your daily routine. Take the stairs instead of the elevator, run small errands on foot or by bike instead of using the car and relax with an evening walk rather than sit in front of the TV. At work, you can do short gymnastic exercises during breaks – you will see that this is not only good for your knee, it also refreshes the mind.

Quote from Christian Krone: "Exercise is essential for osteoarthritis patients because muscle inactivity leads to joint instability, lack of power and getting off axis. And that's why exercise, muscle training and balancing axle situations must be at the forefront to counteract osteoarthritis."

Types of sports
In addition to everyday exercise, regularly doing certain types of sports is ideal for keeping osteoarthritis under control. Swimming, water gymnastics, Nordic Walking, biking or long walks, for example, maintain knee mobility and prevent pain. They also strengthen your leg muscles and promote your mobility and endurance overall. The most important rule is to keep moving, without overexerting yourself. This will have a positive effect on your knee joints, and you'll feel better and more mobile in general.
However, it is better to avoid sports that put a lot of burden on the knee joint due to abrupt stops, tight turns or high pressure at certain points. This includes most ball sports, martial arts or downhill skiing.

Agilium Move: Special training for osteoarthritis of the knee
Get your knee fit: Watch the Agilium Move-Videos featuring special exercises for balance, power and endurance for osteoarthritis of the knee. Our "Agilium Move" programme is designed especially for osteoarthritis patients. It will help you strengthen the muscles in your legs and around the knee joint, increase the stability of your knee joints and become more mobile as a result. Join Christian Neureuther, the former professional skier, and get moving with Agilium Move!
Notice: Your health is important to us. Please take care not to overburden yourself. If in doubt, consult your physician or physiotherapist.





