Anterior knee pain

Causes, symptoms and treatment
Anterior knee pain is generally described as pain around the kneecap. The typical term for it is “patellofemoral pain syndrome” (PFPS). “Patellofemoral” refers to the area between the kneecap (patella) and the thigh bone (femur).
However, PFPS is simply a blanket term for various disorders. The pain can stem from a variety of root causes. Common causes include a condition known as patellar tracking disorder or tendency to dislocation (patella dislocation), also termed patellar lateralisation or patella subluxation. This involves the kneecap slipping out of the femoral groove (dislocation). It can result from an injury to the knee joint or be due to insufficient muscular tension. Arthrosis of the patella can also lead to PFPS. The majority of PFPS patients are young, active women or teenagers. Given the right treatment and appropriate devices, symptoms can often be relieved significantly. In some cases, they disappear entirely.
Ottobock supports and orthoses

What is patellofemoral pain syndrome?
PFPS is a blanket term for various conditions involving the front part of the knee joint, immediately around the patella. The underlying causes can range from malalignment such as patellar tracking disorder up to damaged cartilage. The latter includes patellar chondropathy, chondromalacia and, in the worst-case scenario, retropatellar osteoarthritis (arthrosis of the kneecap).
Chondropathy is the umbrella term for pathological changes in the articular cartilage. These changes can in turn be triggered by various underlying causes of a traumatic, degenerative or inflammatory nature. Chondromalacia is a degenerative disorder affecting the joint cartilage. The cartilage softens, often due to overuse or an injury. This can lead to a loss of cartilage. However, chondropathy and chondromalacia can be reversed in many cases.
Retropatellar osteoarthritis is one of the most severe long-term outcomes. Many people over the age of fifty experience this sort of wear and tear to their kneecaps and cartilage. Arthrosis of the patella is often triggered by an injury, e.g., if the kneecap is broken or dislocated, or after a cruciate ligament injury, or due to a patellar tracking disorder. If your hip and thigh muscles are weak or if your kneecap is not in the right position – for example, too high, too low, or too far to one side – you are more likely to be affected by resulting wear and tear.

Who gets anterior knee pain? And when?
In Germany, more than one in five people are likely to experience anterior knee pain at least once in their life, and sometimes more often. Patellofemoral pain syndrome – arising from patellar tracking disorder, patella dislocation or patella subluxation – is reported to be one of the most common diseases affecting the locomotor system in sports medicine and is the most common cause of knee pain in general. It very often affects young women and teenage girls who regularly engage in sports. Anterior knee pain affects more than twice as many women as men. However, anyone can be affected by patellofemoral pain syndrome. As described above, the cause often lies in weak or shortened thigh muscles. But it can also be triggered by a misaligned kneecap (patella), faulty position of the feet or excessive strain. Experts therefore believe that the pain is the result of a combination of multiple factors.
What happens when you have a patellar tracking disorder?
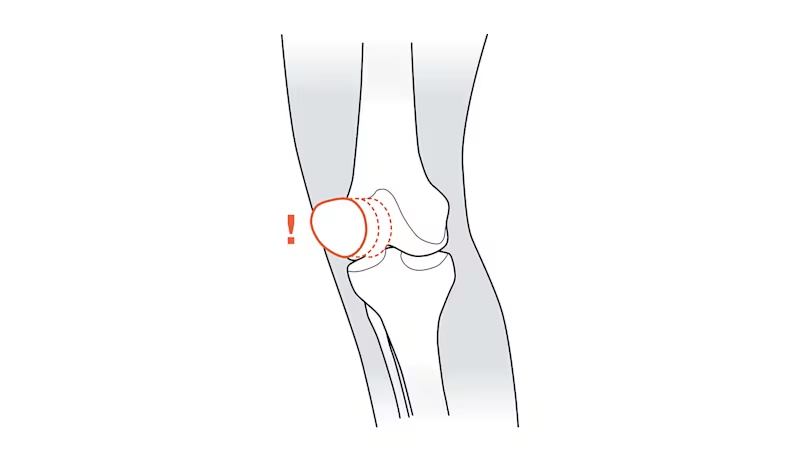
The kneecap (patella) is located above the knee joint and moves most when you bend your knee or extend your leg. It then glides along a special groove on the thigh bone as if on a track. If the patella is misaligned or too much strain or weight is placed on the joint, it can slip out of place, causing irritation between the kneecap and the knee joint. In most cases, the patella slips out of place laterally, in other words, to the outer side of the knee joint. This will generally happen when your leg is bent at an angle between 10° and 30°, because the kneecap is not supported as strongly by bones in this range. Ultimately, this malalignment will result in pain and can lead to patellofemoral pain syndrome or even to dislocation of the patella. The patella is less likely to slip out of place when your knee joint is bent at an angle greater than 30°, because it then rests more firmly in the groove.
Generally speaking, anterior knee pain develops gradually and gets worse particularly when you place external strain on your knee by engaging in sports, climbing stairs, sitting for long periods or bending your knee. When you rest your knee, the pain often subsides again. Given the right therapy, the prognosis for the disease progression is excellent. Sometimes, the anterior knee pain disappears all by itself.
Symptoms of anterior knee pain
The symptoms of patellofemoral pain syndrome can be rather hard to pinpoint. People report pain across the entire anterior knee area, or next to, behind and below the kneecap. At first, the pain is noticeable only when strain or weight is placed on the leg. But as anterior knee pain progresses over a longer period of time, it can become chronic and hurt even when you’re resting. Most people describe it as a stabbing, burning or dull pain in a very specific region, but sometimes the pain can radiate out to the entire anterior knee joint area. Anterior knee pain will generally affect only one knee; it rarely affects both knee joints. As well as feeling pain in the front area of their knee, an increasing number of patients report that they hear a popping noise if they put too much weight on their knee, or a rubbing or catching noise, and that their kneecap feels generally unstable. Symptoms can disappear spontaneously, but some patients find they can persist for years.
Exercises for treating anterior knee pain
In many cases, patellofemoral pain syndrome will improve if you rest your knee joint and adjust your exercise routine. Those affected should avoid movements and sports such as jogging or football, which place excessive strain on the knee. Sports such as swimming, cycling and yoga are good alternatives for people with anterior knee pain. They place less strain on the knee joints and build up the surrounding muscles, which has long-term benefits.
The Ottobock Patella Move programme, an exercise routine developed specifically for people with knee problems, can also support rehabilitation. It helps to reduce pain, build up weak muscles and improve muscle coordination. Another option is physiotherapy. This can improve the kneecap’s range of motion and train your thigh muscles. Strong, flexible quadriceps play an important role in treatment because these muscles are important for stabilising the kneecap.

Therapy that includes sports and exercise is generally very successful. Most patients report that symptoms disappear entirely. Thankfully, surgery is rarely required and is necessary only in a minority of severe and protracted cases, or when the specific problem fails to respond to conservative treatment methods.
If your symptoms are very severe and intense, however, you should rest your knee for a while. In the event of acute symptoms or inflammation, use a cold compress and consider consulting a doctor. Your doctor will feel your knee and may prescribe an MRI, a CT scan or an X-ray to see whether you need to rest the joint for longer, or whether you can safely continue engaging in sports, and whether your pain is possibly caused by another illness. If the joint is inflamed, your doctor may prescribe anti-inflammatory medication such as ibuprofen.

Patella Move therapy programme
3 results out of 3
Orthoses for patellofemoral pain syndrome
A brace such as the Patella Pro can also provide support during therapy for anterior knee pain as well as everyday routines. Studies have shown that orthopaedic devices are proven to help stabilise the knee joint and can even relieve pain. If your patellofemoral pain syndrome is caused by a patellar tracking disorder or tendency to dislocation, your kneecap may tend to shift outwards more easily especially when you bend your leg just slightly. The Ottobock Patella Pro has proven particularly successful here. Using a unique approach, it ensures your kneecap stays in the patellar groove when you bend your leg.

The Patella Pro features a re-alignment mechanism that guides the kneecap securely along the physiological patellar groove and thus prevents it from sliding outwards. By centring the kneecap in the groove, pressure on the cartilage is distributed in a physiological manner across the entire articular surface. The process is completely dynamic because the patella is only aligned as much as the respective movement demands. If you flex your knee joint more, the Patella Pro helps to guide your kneecap back into its natural groove in the femur until it is able to glide smoothly by itself. Within a matter of weeks, you should be able to climb stairs or engage in sports with considerably less pain. To find out more about the ins and outs and benefits of using the Patella Pro re-alignment brace, read the stories from our young users with patellofemoral pain syndrome.

2 results out of 2
Back to everyday activities: three steps to an Ottobock orthosis
- Here you’ll find an overview of all the orthoses and supports that could potentially help you. Take the list with you to your next doctor’s appointment.
- Talk to your doctor about which orthosis is best suited to your symptoms and condition. Your doctor can then write you a prescription for the appropriate orthosis.
- Take your prescription to a medical supply company. They’ll give you your new orthosis and adjust it to fit your exact body measurements.